Hormones are one of the main factors that affect emotion in women. Their bodies go through many stages as they grow older. These changes include puberty, the menstrual cycle, pregnancy, and menopause, which in many cases occur during a person’s "mid-life."
This is a period where women can feel vulnerable and mentally disturbed due to the hormonal imbalance in their body. With that being said, let’s take a look at exactly how hormones influence depression in women.
The link between hormones and depression in women
When hormone levels change due to pregnancy, menopause, or birth control, it can shape up those mood-boosting neurotransmitters. A dip in hormones might lead to less serotonin. This can result in more sadness, anxiety, and irritability.
Testosterone also plays a key role in influencing depression. When it drops, it can bring along some unwelcome side effects such as:
●Depression
●Increased anxiety
●Extra irritability
●A dip in sex drive
●Low energy levels
Possible causes of hormonal depression in women
While research is still going on, experts agree that the following conditions may cause hormonal depression in women.
Premenstrual dysphoric disorder (PMDD)
One of the most important causes is PMDD, or premenstrual dysphoric disorder. It’s like PMS, but on a whole other level.
Symptoms of PMDD can be tough. They include:
●Severe depression or anxiety
●Intense irritability or anger
●Tension
●Mood swings
●Panic attacks
●Losing interest in activities or relationships
●Trouble focusing
●Fatigue
●Food cravings or binge eating
●Difficulty sleeping
●Physical aches and pains
These symptoms often pop up 1 to 2 weeks before your period, when hormone levels start to dip.
PMDD might happen due to increased sensitivity to hormonal changes during the menstrual cycle, including shifts in serotonin levels.

Contraceptives
It’s a well-known fact that hormonal contraceptives can influence mood in women. In a study conducted in 2022, hormonal methods of contraception may contribute to the development of depression eventually. This is due to the amount and type of progesterone in the contraceptives.
Estrogen and progesterone, as well as neurotransmitters like serotonin and dopamine, tend to affect the brain. Estrogen may help protect against mood disorders, while progesterone might worsen them. This is likely because progesterone can lower serotonin levels.
Menopause
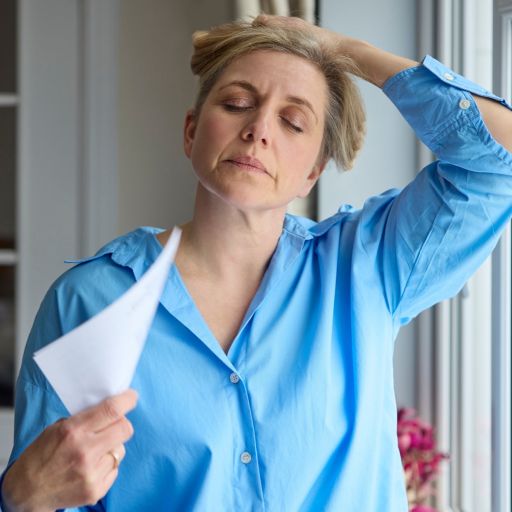
Menopause is also another factor heavily linked with depression. Perimenopause is a time when mood swings can feel like a rollercoaster ride. Sadness and anxiety sneak in as estrogen and progesterone take a nose dive.
Other symptoms of perimenopause, like hot flashes, can disrupt sleep. Poor sleep can increase the likelihood of depression significantly.
Postpartum depression
Allopregnanolone is a neurosteroid, which is a type of steroid present in the brain, synthesized from progesterone. This hormone increases during pregnancy, with the peak coming during the third trimester.
These levels take a sharp dip after finishing childbirth. According to research, this rapid decrease in allopregnanolone levels might be a key factor in developing postpartum depression.
Normally, allopregnanolone levels bounce back a few days after birth. But for some, they don’t. This can lead to those unwelcome feelings of depression.
GABA receptors, the brain’s mood moderators, also get caught in the hormonal chaos.
When hormone levels, especially allopregnanolone, start fluctuating during pregnancy, it can mess with how these receptors work. And just like that, postpartum mental health becomes even more complicated.
Low testosterone
Testosterone deficiency in females may not be the first on the list of symptoms associated with depression. However, it is definitely one of the most important ones and is seldom taken into consideration.
While testosterone is a more dominant male sex hormone, it is present in females as well, though in lesser amounts.
When fluctuations occur, emotional and physical health may be impacted. Less male testosterone can result even in women depression, fatigue, and lack of interest. These symptoms are invisible yet pose an enormous difficulty for mental wellbeing.
Testosterone is known to help control not only mood but also energy levels. This is evidenced by individuals suffering from testosterone imbalances who complain about their mood and energy levels while doing daily activities.
Doctors don’t usually check for low testosterone in women right away, but spotting the connection between low testosterone and depression can make a huge difference in treatment.
The tricky part? Low testosterone is tough to diagnose in women. Its symptoms often get brushed off as stress or a hectic schedule. But once you know low testosterone might be to blame, it opens up new ways to tackle depression and improve overall well-being.

Thyroid problems
Thyroid problems and depression share many symptoms, making their connection confusing. There’s some debate over whether thyroid disorders directly cause depression. A 2021 study suggested the link might not be as strong as previously thought.
Researchers found that subclinical hypothyroidism, where hormone levels are only slightly off, might not be strongly connected to depression. However, overt hypothyroidism, where the thyroid is underactive, could be linked to clinical depression, especially in women.
The connection may come from how thyroid hormones affect the brain and body. These hormones regulate things like metabolism, energy, and mood. When levels are too low, symptoms like fatigue, weight gain, and sadness overlap with depression.
Sex assigned at birth plays a role too. Women are more likely to have thyroid disorders, which might explain the stronger link between hypothyroidism and depression in females. Hormonal changes related to the thyroid can make this relationship even trickier.
While the connection isn’t crystal clear, it’s still important for people with thyroid issues to keep an eye on their mental health. Managing thyroid conditions can help improve both physical and emotional well-being.
Making small lifestyle changes can do wonders for your mood. Especially when dealing with things like PMDD. A little exercise, cutting back on caffeine, and skipping the alcohol can make a big difference. Don't forget about sleep! Quality rest is a must.
Plus, relaxing activities like yoga or meditation can help keep stress in check. But if the blues stick around for more than two weeks, it’s time to call in the pros. A doctor can run hormone tests to check for imbalances.





